August 2023 Case Study
by Nidhi Shah, MD
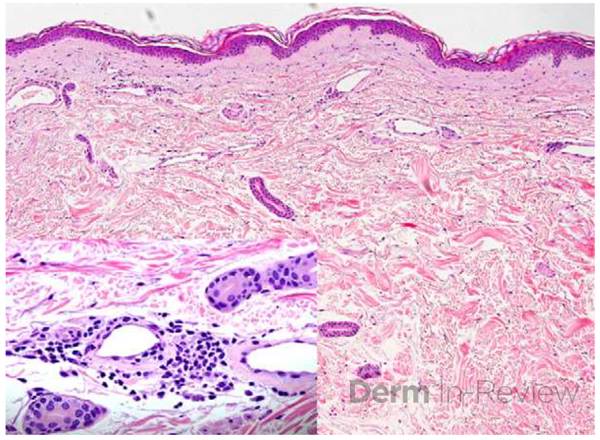
A 67-year-old male with past medical history of hypertension, type 2 diabetes, cirrhosis, and psoriasis presented for a pruritic rash involving his scalp, trunk, and extremities for a year. On examination, patient had small erythematous macules and telangiectasias scattered on the trunk, extremities, and scalp (Figure 1). A punch biopsy of the left lower back was obtained (Figure 2)1. Laboratory findings demonstrated an elevated tryptase level.
Based on the clinical presentation and biopsy and laboratory findings, what is the next best test?
A.) CK
B.) Hepatitis panel
C.) c-KIT
D.) TSH
E.) HIV

Correct Answer: C.) c-KIT
Explanation of Correct Answer:
Patient’s telangiectatic and macular rash with biopsy findings of mononuclear infiltrate of mast cells around the capillaries in the upper dermis raises concerns for telangiectasia macularis eruptive perstans (TMEP), a rare form of cutaneous mastocytosis. TMEP most commonly manifests in adulthood, although rare reports of pediatric cases have been reported.1,2 Although previously considered to be a solely cutaneous disease, recent evidence suggests the presence of systemic involvement including bone marrow, gastrointestinal tract, liver, spleen and lymph node.2,3
TMEP classically presents as small, irregular red-brown blanchable telangiectatic macules ranging from 2-4mm in diameter overlying a tan background.2 These lesions generally are non-pruritic and involve the trunk and proximal extremities in a symmetric pattern, sparing the palms, soles, and face in most cases. Commonly positive in urticaria pigmentosum or maculopapular cutaneous mastocytosis (UP/MPCP), Darier’s sign is usually negative or slight in TMEP given the low number of mast cells involved.2
If characteristic skin lesions are accompanied by symptoms like flushing, diarrhea, dyspnea, tachycardia, pruritis, syncope, or indications of anaphylaxis, it’s important to consider the possibility of systemic involvement.2 Serum tryptase and 24-hour urine histamine levels are used as preliminary test to investigate for systemic involvement with tryptase levels >20 µg/L concerning for systemic mastocytosis.2 In adults, a c-KIT proto-oncogene mutation is most commonly observed which leads to mast cell hyperplasia.4 The type III transmembrane tyrosine kinase receptor c-kit has an extracellular domain that binds to mast cell growth factor and activation leads to mast cell growth and production.2 Although the mutation is not present in all patients, proto-oncogene alternations may be correlated with more aggressive systemic involvement, making it important to check for the mutation.4
There is no gold standard treatment for TMEP and treatment is based upon the type of systemic involvement and clinical symptoms. Lifestyle modifications to avoid stimulation of mast cell degranulation such as exposure to sunlight and extreme temperatures, alcohol, and drugs should be practiced. Additional treatment modalities include antihistamines, PUVA, and narrow-band UVB.2,4 Beyond management of symptoms, staging studies are required to evaluate for aggressive disease. The only FDA approved treatment for cytoreduction in mastocytosis is avapritinib, an oral small molecule inhibitor of D816V-mutant KIT.5
References
- Martín-Fuentes A, Pastor-Nieto MA, De Eusebio-Murillo E. Telangiectatic Macules in a 90-Year-Old Woman. Actas Dermo-Sifiliográficas (English Edition). 2012;103(1):65-66. doi:10.1016/j.adengl.2011.07.006
- Watkins CE, Bokor WB, Leicht S, Youngberg G, Krishnaswamy G. Telangiectasia Macularis Eruptiva Perstans: more than skin deep. Dermatol Reports. 2011;3(1):e12. doi:10.4081/dr.2011.e12
- Severino M, Chandesris MO, Barete S, et al. Telangiectasia macularis eruptiva perstans (TMEP): A form of cutaneous mastocytosis with potential systemic involvement. J Am Acad Dermatol. 2016;74(5):885-891.e1. doi:10.1016/j.jaad.2015.10.050

