March 2023 Case Study
by Emily Murphy, MD1
- Department of Dermatology, George Washington University School of Medicine and Health Sciences
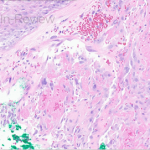
A 70-year-old healthy male presented with a chronic wound on his scalp that started 4 months ago. On examination, a 2.5-centimeter circular, ulcerated violaceous plaque with hemorrhagic crusting was present on the scalp (figure 1). A punch biopsy of the raised border was done (figure 2a, hematoxylin-eosin staining). The atypical cells stained positively for erythroblast transformation specific related gene (ERG) and CD31.
Based on the clinical presentation and biopsy findings, which two patients would be least likely to develop the same malignancy as the above patient?
A.) 80-year-old male with a plaque on the cheek
B.) 35-year-old male with a tumor that also stained positively for HHV-8
C.) 65-year-old male exposed to vinyl chloride for many years in his occupation
D.) 50-year-old woman with a lower limb plaque after treatment of a uterine carcinoma 10 years prior
E.) 55-year-old woman with a plaque on the scalp who reports chronic sun exposure and many blistering sunburns
F.) 40-year-old woman who had radiation for breast cancer 5 years ago
- Figure 1 – Clinical Photo
- Figure 2a – H&E
- Figure 2a – IHC stain
Correct Answer: B, E
Given the biopsy revealed proliferation of atypical and inter-anastomosing vascular channels along with increased mitotic figures, and that these atypical cells were positive for ERG and CD31, the patient was diagnosed with angiosarcoma, a rare soft tissue sarcoma, with only about 200 reported cases in the United States per year.1 These tumors present on the skin as a purpura-like or violaceous papules to plaques, that are often multifocal.2 As the tumors grow, ulceration and hemorrhage often occur, as was seen in this case.2
The cutaneous form of angiosarcoma most often occurs spontaneously, typically in elderly men on the head and neck (choice A).2 The scalp is a particularly common site, as in our patient, and is also associated with a poor prognosis.3,4 Angiosarcomas can also occur secondary to radiation (choice F) or chronic lymphedema (choice D), which is called Stewart-Treves syndrome.1,2 Stewart-Treves can be seen after lymph node dissection in setting of breast cancer (upper limb) or uterine cancer (lower limb, choice D).1 In cases of radiation or lymphedema, the tumor often develops at least 5 years later.1,2 Angiosarcoma can also be seen with chronic exposure to various toxins including vinyl chloride, arsenic, thorium dioxide, and anabolic steroids (choice C).2 Unlike Kaposi sarcoma, HHV-8 is not associated with angiosarcoma (choice B).6 Further, in contrast to many other cutaneous cancers, sun exposure is not associated with angiosarcomas (choice E).7
Prior to treatment, an MRI of the primary lesion should be done to evaluate the extent of disease, as well as a CT chest to rule of pulmonary disease, which is the most common site of metastasis.1,2 A PET scan may also be done to exclude other sites of metastasis.2 Given the rarity of these tumors, standard treatment algorithms do not exist. For local disease, wide local excision is done, typically followed by surgical site radiation of at least 50 gray.1 For unresectable or metastatic disease, chemotherapy, often paclitaxel, is used in combination with radiation.1 Clinical trials are currently examining the impact of immunotherapy on angiosarcoma as well. Despite treatment, these tumors often recur, leading to a 5-year survival less than 40%.1
References
- Fujisawa Y, Yoshino K, Fujimura T, et al. Cutaneous Angiosarcoma: The Possibility of New Treatment Options Especially for Patients with Large Primary Tumor. Front Oncol. 2018;8:46. doi:10.3389/fonc.2018.00046
- Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ. Angiosarcoma. Lancet Oncol. 2010;11(10):983-991. doi:10.1016/S1470-2045(10)70023-1
- Ramakrishnan N, Mokhtari R, Charville GW, Bui N, Ganjoo K. Cutaneous Angiosarcoma of the Head and Neck-A Retrospective Analysis of 47 Patients. Cancers (Basel). 2022;14(15):3841. doi:10.3390/cancers14153841
- Shin JY, Roh SG, Lee NH, Yang KM. Predisposing factors for poor prognosis of angiosarcoma of the scalp and face: Systematic review and meta-analysis. Head Neck. 2017;39(2):380-386. doi:10.1002/hed.24554
- Jennings TA, Peterson L, Axiotis CA, Friedlaender GE, Cooke RA, Rosai J. Angiosarcoma associated with foreign body material. A report of three cases. Cancer. 1988;62(11):2436-2444. doi:10.1002/1097-0142(19881201)62:11<2436::aid-cncr2820621132>3.0.co;2-j
- Schmid H, Zietz C. Human herpesvirus 8 and angiosarcoma: analysis of 40 cases and review of the literature. Pathology. 2005;37(4):284-287. doi:10.1080/00313020500169495
- North P. Vascular Neoplasms and Neoplastic-Like Proliferations. In: Dermatology. Fourth Edition. Elsevier; :2020-2049. Accessed February 18, 2023. https://www-clinicalkey-com.proxygw.wrlc.org/#!/content/book/3-s2.0-B9780702062759001148?scrollTo=%23top