October 2021 Case Study
by Emily Murphy, MD, Karl Saardi, MD
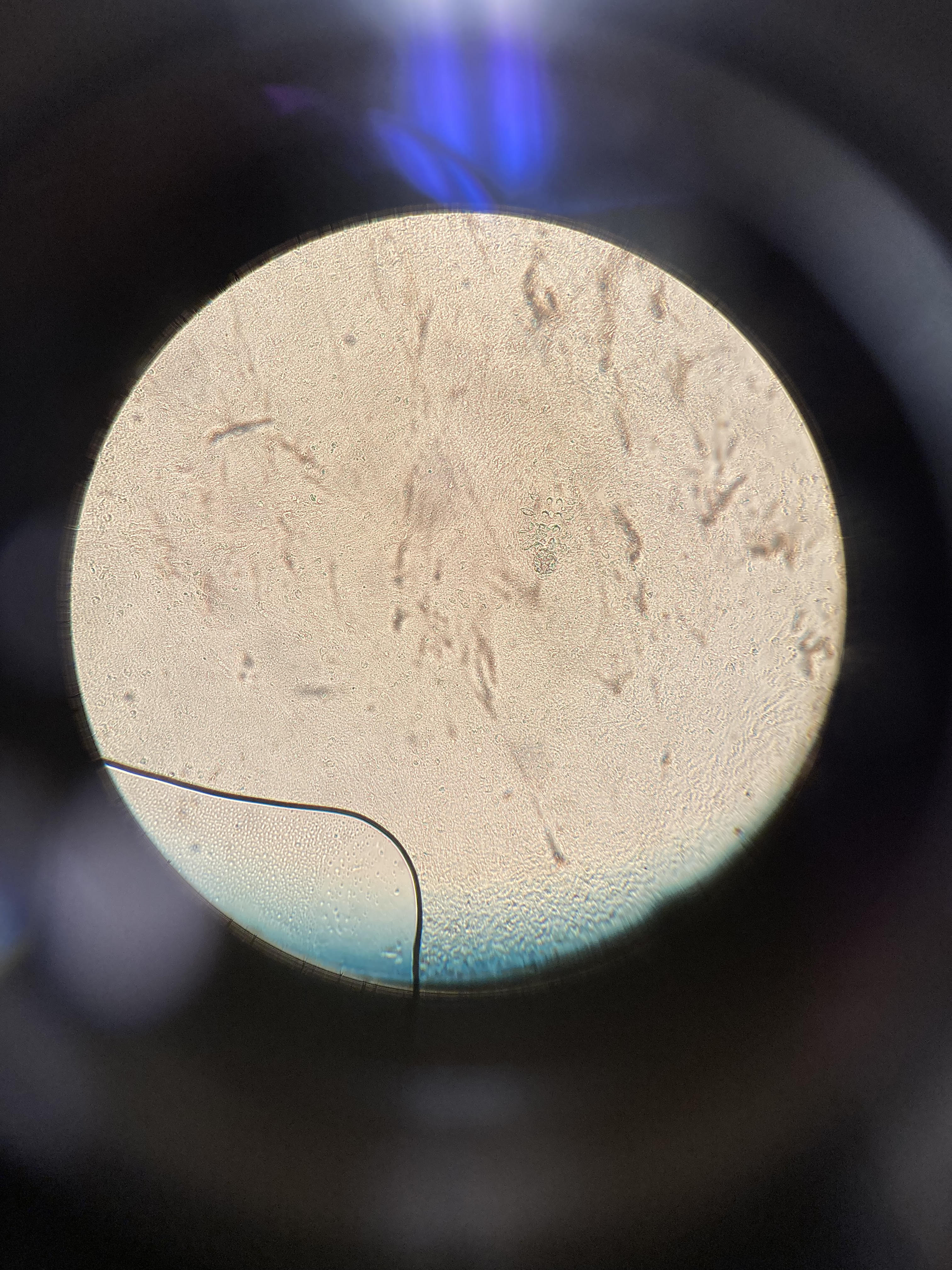
A 38-year-old male with a past medical history of HIV presented with an intermittent, itchy rash for 1.5 years. The rash first occurred on his upper arms but now predominantly affects his upper back. He has not tried any therapies (figure 1). Of note, he was off anti-retroviral therapy (ART) for several years resulting in a low CD4 count of 15. He restarted ART three months prior to presentation but this did not affect the course of his rash. One of the pustules was de-roofed and examined after application of potassium hydroxide (figure 2).
Which of the following statements is true about this eruption?
A.) This disease is more likely in patients with HIV regardless of CD4 count.
B.) While potassium hydroxide staining of skin scrapings may help with the diagnosis, the pathogen is only rarely seen on microscopy.
C.) This eruption can be seen as part of immune inflammatory reconstitution syndrome.
D.) Compared to this eruption, papular pruritic eruption of HIV has a similar clinical appearance and distribution on the face, neck, and trunk.
E.) One possible treatment is a two week course of Ivermectin.
Correct Answer: C
Explanation/Literature review:
The demodex mite is a normal colonizer of the skin; 69% of patients aged 31 to 50 years old are colonized and 95% of patients over 71 years old are colonized.1 Demodex folliculitis occurs when there is inflammation of pilosebaceous units infested with mites. Bacterial antigens on the mites trigger a lymphocytic infiltrate, producing the erythematous perifollicular papules and pustules that are seen with this disease.1 The disease tends to occur on the face and neck but can be more diffuse.1 A skin scraping or de-roofing of a pustule and staining with potassium hydroxide will usually reveal the demodex mite on microscopy (answer B).1,2 There are two types of mites. Demodex folliculorium is the larger mite that is often present on the face, clustered in groups of 10-15 mites on the follicular infundibulum. Demodex brevis is the smaller mite that often exists on the trunk as a solitary mite in the sebaceous gland.1
Demodex folliculitis is more common in immunosuppressed patients, especially patients with HIV who have a CD4 count less than 200 (answer A).1,2 Immunosuppressed patients may have more diffuse disease involving the sebaceous areas of the face, upper chest, and interscapular back.1,2 While demodex folliculitis is often seen with low CD4 counts, it can also paradoxically occur with immune reconstitution inflammatory syndrome, when patients have an increasing CD4 count after starting ART (answer C).2 This phenomenon may be due to uncontrolled replication of the mites or a local influx of T cells with immune reconstitution.2 Demodex folliculitis can be seen with other immunosuppressed patients, including patients with leukemia who undergo stem cell transplant, where this eruption can mimic acute graft versus host disease.3
Beyond demodex folliculitis, other diseases should be considered when a patient with HIV presents with pruritic papules and pustules, including papular pruritic eruption of HIV, immunosuppression-associated eosinophilic folliculitis, and pityrosporum folliculitis. These four eruptions are morphologically similar but the distribution of papular pruritic eruption of HIV differs, often presenting on the extremities, rather than the face, neck, and upper trunk in the other three diseases (answer D).1,3,4
Demodex folliculitis can be treated topically or orally, with the goal of reducing the demodex mite infestation. Response to therapy confirms pathogenicity of the mite.1 Topical treatments include sulfur products like sodium sulfacetamide 10% lotion or shampoo, ivermectin 1% cream, permethrin 5% cream, or metronidazole 1% cream/gel.1,5 More diffuse or recalcitrant disease should be treated orally with a single dose of ivermectin 200 micrograms/kilogram (12-15 milligrams) (answer E).1,5 Initial oral therapy can be followed by intermittent topical therapy to minimize the long-term population of demodex mites.
References
- Elston CA, Elston DM. Demodex mites. Clin Dermatol. 2014;32(6):739-743. doi:10.1016/j.clindermatol.2014.02.012
- Delfos NM, Collen AFS, Kroon FP. Demodex folliculitis: a skin manifestation of immune reconstitution disease. AIDS. 2004;18(4):701-702. doi:10.1097/00002030-200403050-00019
- Cotliar J, Frankfurt O. Demodex folliculitis mimicking acute graft-vs-host disease. JAMA Dermatol. 2013;149(12):1407-1409. doi:10.1001/jamadermatol.2013.5891
- Motswaledi MH, Visser W. The spectrum of HIV-associated infective and inflammatory dermatoses in pigmented skin. Dermatol Clin. 2014;32(2):211-225. doi:10.1016/j.det.2013.12.006
- Jacob S, VanDaele MA, Brown JN. Treatment of Demodex-associated inflammatory skin conditions: A systematic review. Dermatol Ther. 2019;32(6):e13103. doi:10.1111/dth.13103