June 2020 Case Study
A 41-year-old female presents to clinic with four weeks of “breakouts” on her cheeks. She reports she has been suffering with worsening burning and stinging of the face, which she attributes to her sensitive skin. She has been using waterless moisturizing cream based washes to cleanse nightly, otherwise she denies any new products. Examination reveals the findings shown here.
What is your next best step?
A) Start adapalene 0.1% gel three nights a week, gradually increasing to nightly
B) Order serum antinuclear antibody testing
C) Obtain scraping of skin surface
D) Obtain bacterial culture of intact pustule
E) Order serum ACE levels
F) Start doxycycline 100mg twice daily
Correct Answer: C) Obtain scraping of skin surface
A) Incorrect. This answer implies that the patient is suffering from comedonal acne. While the selection of adapalene 0.1% gel takes into account the patient’s self –reported sensitivity, and there are some scattered hyperpigmented macules concerning for post-inflammatory hyperpigmentation, the lesions not comedonal.
B) Incorrect. This answer implies that the suspected diagnosis is systemic lupus erythematosus. While the malar rash of acute cutaneous lupus can present with centrofacial erythema and have some associated sensitivity, it is generally more confluent and widespread, sparing the nasolabial folds and lacks pustules.
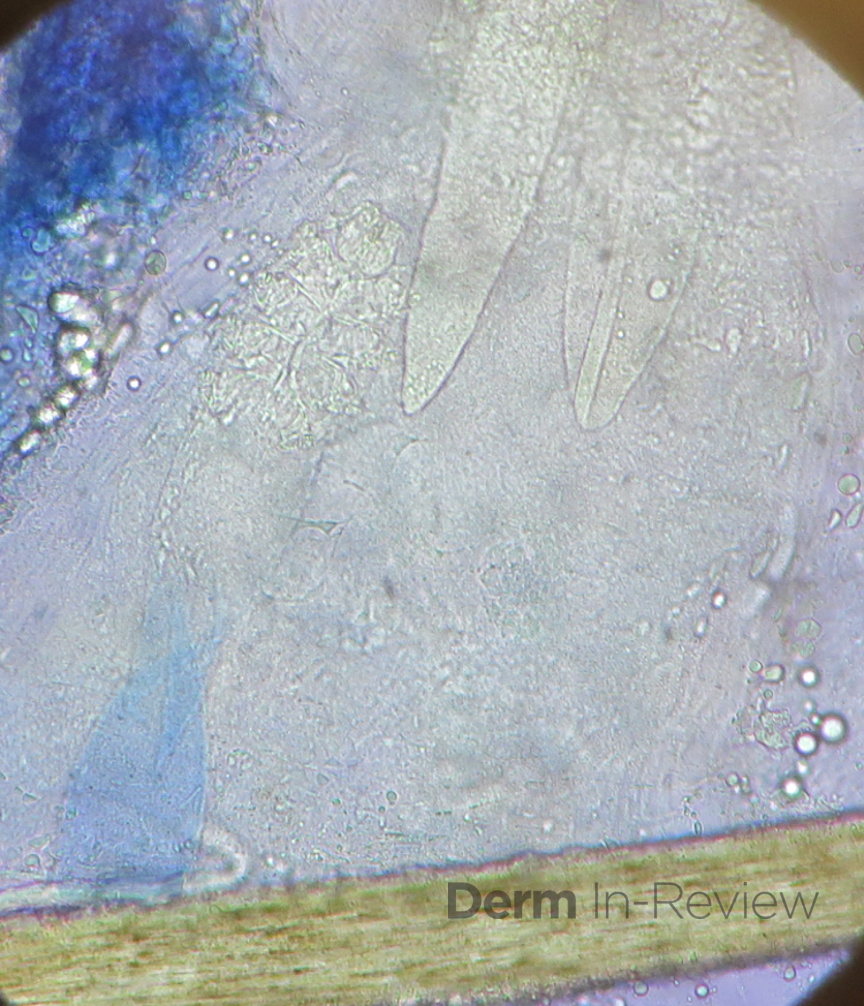
C) Correct. The clinical presentation shown is consistent with a demodex dermatitis, which includes small monomorphic erythematous papulopustules, and gentle scraping of the skin will reveal Demodex mites on KOH prep.
D) Incorrect. Although gram-negative folliculitis can present with eruptive pustules in the facial T-zone in a perinasal distribution, it is usually seen in patients with acne vulgaris receiving long-term antibiotic therapy (which is not the case in this patient).
E) Incorrect. This answer implies a suspected diagnosis of sarcoidosis, which can present with erythema and papules and can be mistaken for rosacea. It would not present with pustules, as in this case.
F) Incorrect. This answer implies a suspected diagnosis of rosacea. Although rosacea can present with papules and pustules superimposed on an erythematous background, there is no appreciable fixed centrofacial erythema, scleral injection, phymatous changes, or facial edema. It is important to note that erythema and telangiectasias can be difficult to discern in the setting of increased background pigmentation, and dermoscopy can be a useful tool to help identify telangiectasias. Also of note, post-inflammatory hyperpigmentation is almost never directly related to rosacea (unless the disease is very chronic and severe or the patient has injured skin inadvertently in an attempt to treat via picking or topical therapies).1
This month’s case study represents a case of demodex dermatitis, with KOH findings as shown below:
Demodex folliculorum is a vermiform mite that inhabits the pilosebaceous units of the face, most notably the forehead, cheeks, nasolabial folds and nose because of the high density of sebaceous glands in these areas.2 Demodex mites have been associated with various inflammatory eruptions including demodectic blepharitis, demodectic folliculitis, demodectic abscess, demodectic alopecia and rosacea-like lesions.3 Demodex mites do not regularly induce illness in healthy hosts aside from eruptions on the face. Severe, problematic eruptions have been associated with patients suffering from myelocytic leukemia, HIV, or diabetes.2
Recent literature review and meta-analysis revealed that patients with rosacea had significantly higher prevalence and degrees of Demodex mite infestation than did control patients, and it has been hypothesized that Demodex mites may play a role in both erythematotelangiectatic rosacea and papulopustular rosacea.4 Antiparasitic agents have been used for treatment of rosacea based on the possible role of cutaneous demodicosis with promising results in papulopustular rosacea.5
Diagnosis of demodex dermatitis involves skin scraping and KOH prep/microscopy. Treatment options include topical permethrin, sulfur, lindane, benzyl benzoate, or benzoyl peroxide. Oral ivermectin and metronidazole have also been studied as treatment options.3
References
- Huerth K. Rosacea: Nuances in Clinical Presentation and Treatment. Review of the 2019 Skin of Color Update Lecture by Fran Cook-Bolden, MD. Next Steps in Dermatology. https://nextstepsinderm.com/derm-topics/skin-of-color/rosacea-nuances-in-clinical-presentation-and-treatment/
- Elston CA, Elston DM. Demodex mites. Clinics in Dermatology. 2014 32, 739-743.
- James W, Elston J, Treat J. Parasitic Infections, Stings, and Bites. In: Andrews’ Diseases of the Skin. 13th Elsevier.
- Chang YS, Huang YC. Role of Demodex Mite Infestation in Rosacea: A Systematic Review and Meta-Analysis. J Am Acad Dermatol. 2017 Sep;77(3):441-447.e6.
- Stein L, Kircik L, Fowler J et al. Efficacy and safety of ivermectin 1% cream in treatment of papulopustular rosacea: results of two randomized, double-blind, vehicle-controlled pivotal studies. J Drugs Dermatol. 2014;13(3):316-323.